A long-term care plan helps people with disabilities thrive : Shots


Courtney Johnson, who has autism and multiple chronic illnesses, lives relatively independently. Her grandparents and friends have helped her access social services. Still, she says, “thinking about the future is a bit terrifying to me.”
Tristan Lane
hide caption
toggle caption
Tristan Lane
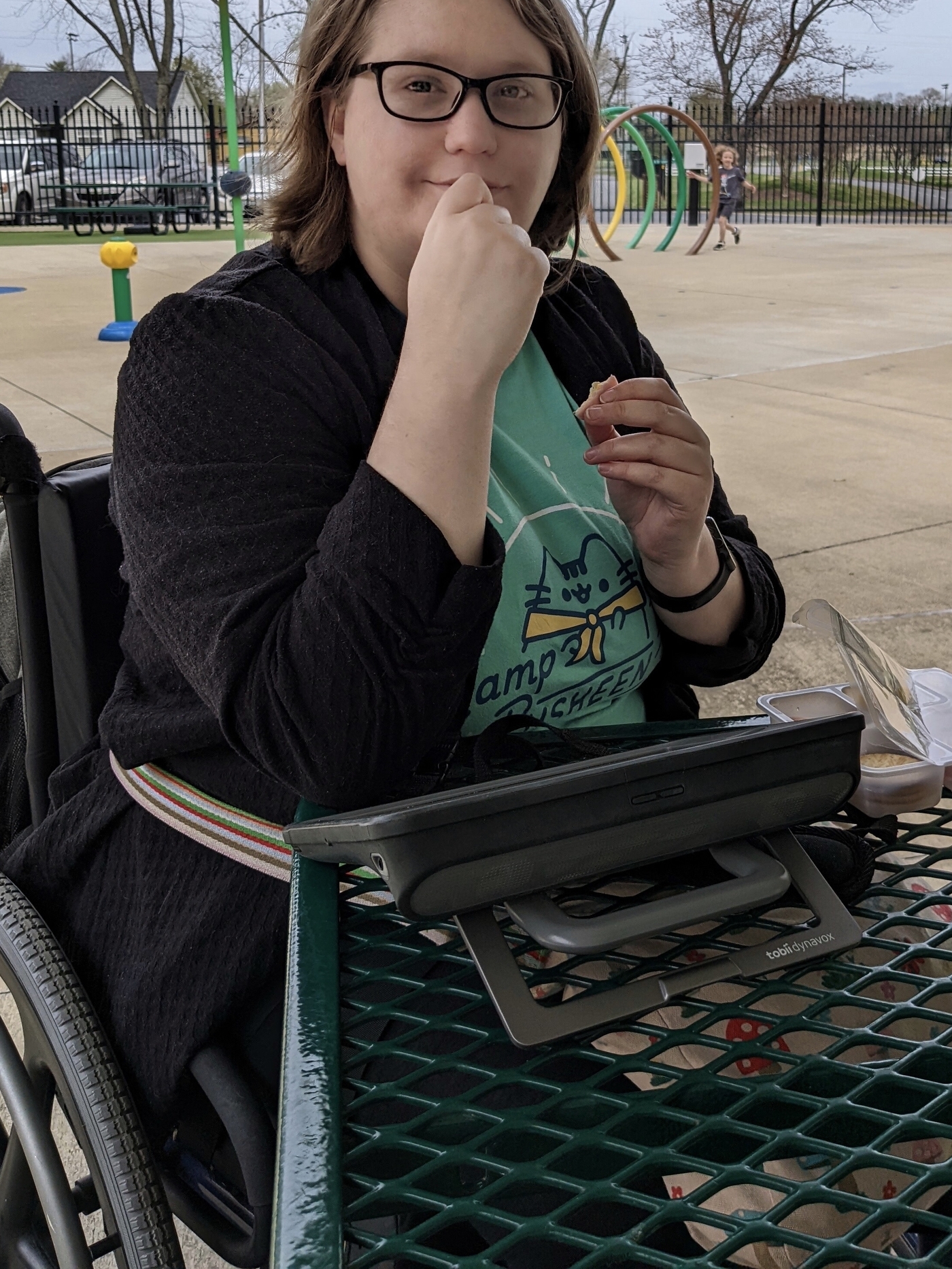
Courtney Johnson, who has autism and multiple chronic illnesses, lives relatively independently. Her grandparents and friends have helped her access social services. Still, she says, “thinking about the future is a bit terrifying to me.”
Tristan Lane
Thinking about the future makes Courtney Johnson nervous.
The 25-year-old blogger and college student has autism and several chronic illnesses, and with the support of her grandparents and friends, who help her access a complex network of social services, she lives relatively independently in Johnson City, Tenn.
“If something happens to them, I’m not certain what would happen to me, especially because I have difficulty with navigating things that require more red tape,” she says.
Johnson says she hasn’t made plans that would ensure she receives the same level of support in the future. She especially worries about being taken advantage of or being physically harmed if her family and friends can’t help her — experiences she’s had in the past.
“I like being able to know what to expect, and thinking about the future is a bit terrifying to me,” she says.
Johnson’s situation isn’t unique.
25{b574a629d83ad7698d9c0ca2d3a10ad895e8e51aa97c347fc42e9508f0e4325d} of U.S. adults live with a disability
Experts say many people with intellectual and developmental disabilities do not have long-term plans for when family members lose the ability to help them get access to government services or to care for them directly.
Families, researchers, government officials, and advocates worry that the lack of planning — combined with a social safety net that’s full of holes — has set the stage for a crisis in which people with disabilities can no longer live independently in their communities. If that happens, they could end up stuck in nursing homes or state-run institutions.
“There’s just potential for a tremendous human toll on individuals if we don’t solve this problem,” says Peter Berns, CEO of the Arc of the United States, a national disability-rights organization.

About 25{b574a629d83ad7698d9c0ca2d3a10ad895e8e51aa97c347fc42e9508f0e4325d} of adults in the U.S. live with a disability, according to the Centers for Disease Control and Prevention. Nearly 75{b574a629d83ad7698d9c0ca2d3a10ad895e8e51aa97c347fc42e9508f0e4325d} of Americans with disabilities live with a family caregiver, and about 25{b574a629d83ad7698d9c0ca2d3a10ad895e8e51aa97c347fc42e9508f0e4325d} of those caregivers are 60 or older, according to the Center on Developmental Disabilities at the University of Kansas.
Any care plan needs to be ‘a living document, because things change’
But only about half of families that care for a loved one with disabilities have made plans for the future, and an even smaller portion have revisited those plans to ensure they’re up to date, says Meghan Burke, an associate professor of special education at the University of Illinois in Urbana-Champaign.
“Engaging in it once is good, right? But you can’t only engage in it once,” she says. “It’s a living document, because things change, people change, circumstances change.”
Burke’s research has found several barriers to planning for the future: financial constraints, reluctance to have hard conversations, trouble understanding government services. Creating plans for people with disabilities also is a complex process, with many questions for families to answer: What are their relatives’ health needs? What activities do they enjoy? What are their wishes? Where will they live?

Rob Stone was born with a condition that restricts much of his movement. His mother, Jeneva, says her family has been “flummoxed” by the process of planning for the future. They just want to make sure Rob will have a say in where he lives and the care he receives.
rahfoard
hide caption
toggle caption
rahfoard

Rob Stone was born with a condition that restricts much of his movement. His mother, Jeneva, says her family has been “flummoxed” by the process of planning for the future. They just want to make sure Rob will have a say in where he lives and the care he receives.
rahfoard
Burke has firsthand experience answering those questions. Her younger brother has Down syndrome, and she expects to become his primary caregiver in the future — a situation she said is common and spreads the work of caregiving.
“This is an impending intergenerational crisis,” she said. “It’s a crisis for the aging parents, and it’s a crisis for their adult offspring with and without disabilities.”
Nicole Jorwic, chief of advocacy and campaigns for Caring Across Generations, a national caregiver advocacy organization, says the network of state and federal programs for people with disabilities can be “extremely complicated” and is full of holes. She has witnessed those gaps as she has helped her brother, who has autism, get access to services.
“It’s really difficult for families to plan when there isn’t a system that they can rely on,” she says.
Advocates see a chronic underinvestment in Medicaid disability services
Medicaid pays for people to receive services in home and community settings through programs that vary state to state. But Jorwic says there are long waitlists. Data collected and analyzed by KFF shows that queue is made up of hundreds of thousands of people across the country. Even when people qualify, Jorwic adds, hiring someone to help can be difficult because of persistent staff shortages.
Jorwic says more federal money could shorten those waitlists and boost Medicaid reimbursements to health care providers, which could help with workforce recruitment. She blames chronic underinvestment in Medicaid disability services for the lack of available slots and a dearth of workers to help people with disabilities.
“It’s going to be expensive, but this is four decades of funding that should have been done,” she says.


Congress recently put about $12.7 billion toward enhancing state Medicaid programs for home- and community-based services for people with disabilities, but that money will be available only through March 2025. The Build Back Better Act, which died in Congress, would have added $150 billion, and funding was left out of the Inflation Reduction Act, which became law this summer, to the disappointment of advocates.
Jeneva Stone’s family in Bethesda, Md., has been “flummoxed” by the long-term planning process for her 25-year-old son, Rob. He needs complex care because he has dystonia 16, a rare muscle condition that makes moving nearly impossible for him.
“No one will just sit down and tell me what is going to happen to my son,” she says. “You know, what are his options, really?”
A special savings account and plan in place for ‘supported decision-making’
Stone says her family has done some planning, including setting up a special needs trust to help manage Rob’s assets and an ABLE account, a type of savings account for people with disabilities. They’re also working to give Rob’s brother medical and financial power of attorney and to create a supported decision-making arrangement for Rob to make sure he has the final say in his care.
“We’re trying to put that scaffolding in place, primarily to protect Rob’s ability to make his own decisions,” she says.

Alison Barkoff is acting administrator for the Administration for Community Living, part of the U.S. Department of Health and Human Services. Her agency recently released what she called a “first ever” national plan, with hundreds of actions the public and private sectors can take to support family caregivers.
“If we don’t really think and plan, I’m concerned that we could have people ending up in institutions and other types of segregated settings that could and should be able to be supported in the community,” says Barkoff, who notes that those outcomes could violate the civil rights of people with disabilities.
She says her agency is working to address the shortages in the direct care workforce and in the supply of affordable, accessible housing for people with disabilities, as well as the lack of disability-focused training among medical professionals.

Evan Woody has needed round-the-clock care since his brain injury and lives with his parents in Dunwoody, Ga. His father, Philip, says his family has some plans in place for Evan’s future, but one question is still unanswered: Where will Evan live when he can no longer live with his parents?
Philip Woody
hide caption
toggle caption
Philip Woody

Evan Woody has needed round-the-clock care since his brain injury and lives with his parents in Dunwoody, Ga. His father, Philip, says his family has some plans in place for Evan’s future, but one question is still unanswered: Where will Evan live when he can no longer live with his parents?
Philip Woody
But ending up in a nursing home or other institution might not be the worst outcome for some people, says Berns, who points out that people with disabilities are overrepresented in jails and prisons.
A step-by-step guide to coming up with the right plan
Berns’ organization, the Arc offers a step-by-step planning guide and has compiled a directory of local advocates, lawyers, and support organizations to help families. Berns says that making sure people with disabilities have access to services — and the means to pay for them — is only one part of a good plan.
“It’s about social connections,” Berns says. “It’s about employment. It’s about where you live. It’s about your health care and making decisions in your life.”
Philip Woody feels as though he has prepared pretty well for his son’s future. Evan, 23, lives with his parents in Dunwoody, Ga., and needs round-the-clock support after a fall as an infant resulted in a significant brain injury. His parents provide much of his care.
Woody says his family has been saving for years to provide for his son’s future, and Evan recently got off a Medicaid waitlist and is getting support to attend a day program for adults with disabilities. He also has an older sister in Tennessee who wants to be involved in his care.
But two big questions are plaguing Woody: Where will Evan live when he can no longer live at home? And will that setting be one where he can thrive?
“As a parent, you will take care of your child as well as you can for as long as you can,” Woody says. “But then nobody after you pass away will love them or care for them the way that you did.”
KHN (Kaiser Health News) is a national, editorially independent program of the Kaiser Family Foundation (KFF).